MOBILE TRANSFER OF 12-CHANNEL-ECG FROM EMERGENCY PHYSICIAN TO HOSPITAL
Even modest delays in diagnosing and treating myocardial infarctions can significantly impact mortality. Several studies have shown that the transmission of a 12-channel-ECG prior to arrival at the hospital can compress this delay and improve survival.
(ESC Guidelines on Acute and Chronic Heart Failure)
The mobile ECG-system CREMONI® (Cardiac & REspiratory MONItoring) is the worldwide first and only telemonitor being able to transfer a complete, high-quality 12-channel-ECG with only four electrodes in real time using an integrated GSM-technology. The data can be transferred to a medical center anytime. The small CREMONI® recognizes myocardial ischemia and cardiac arrhythmias. It contains a modern signal processing-, mobile phone- and computer-technology.
In a network between hospital and emergency services, the ambulances are equipped with at least one CREMONI-telemonitor. A computer with the special software CREMONI-Soft, located in the department of cardiology or the center of the emergency service, can receive anytime a 12-channel-ECG, which is transmitted by one of the connected CREMONI-telemonitors. Each transmitted ECG is digitally archived.
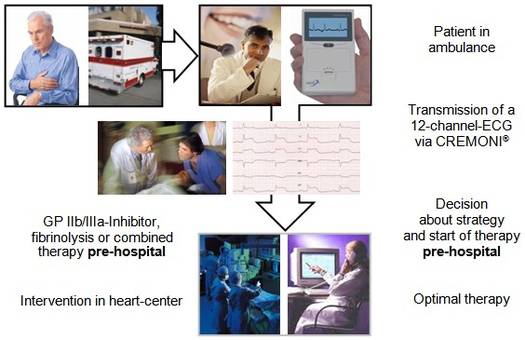
PRE-HOSPITAL DIAGNOSIS IN ACS LEADS TO PRE-HOSPITAL START OF THERAPY
If the mobile ECG-system CREMONI is used in the ambulance, the emergency physician is always connected with a cardiologist. In patients with suspicion of an acute coronary syndrome ischemic events and arrhythmias can be detected.By mobile phone, the emergency physician can present the patient to a hospital based ECG surveillance center, which is served by experienced cardiologists.
The cardiologist can see immediately the 12-channel-ECG on the computer screen. The computer for the ECG-transmission can be located in the ICU, in the cathlab or in the center of the emergency service. The emergency physician and the cardiologist can decide about the optimal reperfusion strategy and the therapy. Even in the ambulance the emergency physician can start the pharmacologic treatment (GP IIb/IIIa-inhibitor and/or thrombolysis) and the cardiologist can prepare the cathlab for an acute coronary intervention.
Complications caused by combinations of drugs (for example full-dose thrombolysis and GP IIb/IIIa-inhibitor) can be avoided.
Also in cases with short distances to the hospital, the pre-hospital arrangement helps to avoid time-intensive detours in the hospital (for example direct transfer the intensive care unit or to the cathlab).
Target groups of this new technology are patients with an acute coronary syndrome as well as patients with suspicion of an acute coronary syndrome. Due to the early recognition of ischemia, more patients can get effective drugs and if necessary interventional therapy – and many of them get the therapy earlier.